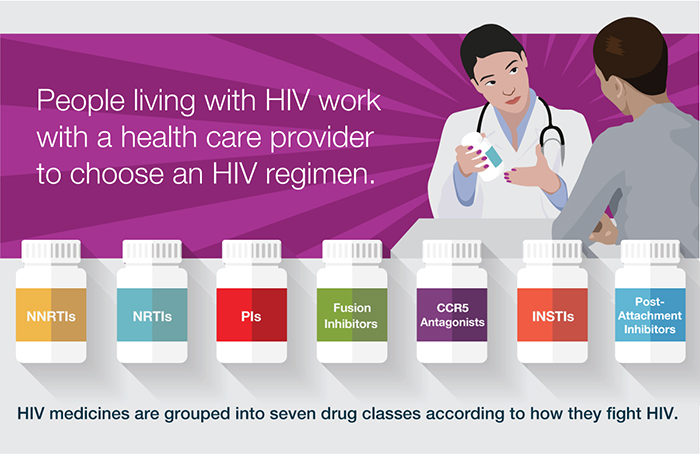
| Nucleoside Reverse Transcriptase Inhibitors (NRTIs) |
| NRTIs block reverse transcriptase, an enzyme HIV needs to make copies of itself. |
abacavir
(abacavir sulfate, ABC) |
Ziagen |
December 17, 1998 |
emtricitabine
(FTC) |
Emtriva |
July 2, 2003 |
lamivudine
(3TC) |
Epivir |
November 17, 1995 |
tenofovir disoproxil
fumarate
(tenofovir DF, TDF) |
Viread |
October 26, 2001 |
zidovudine
(azidothymidine, AZT, ZDV) |
Retrovir |
March 19, 1987 |
| Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs) |
| NNRTIs bind to and later alter reverse transcriptase, an enzyme HIV needs to make copies of itself. |
doravirine
(DOR) |
Pifeltro |
August 30, 2018 |
efavirenz
(EFV) |
Sustiva |
September 17, 1998 |
etravirine
(ETR) |
Intelence |
January 18, 2008 |
nevirapine
(extended-release nevirapine, NVP) |
Viramune |
June 21, 1996 |
| Viramune XR (extended release) |
March 25, 2011 |
rilpivirine
(rilpivirine hydrochloride, RPV) |
Edurant |
May 20, 2011 |
| Protease Inhibitors (PIs) |
| PIs block HIV protease, an enzyme HIV needs to make copies of itself. |
atazanavir
(atazanavir sulfate, ATV) |
Reyataz |
June 20, 2003 |
darunavir
(darunavir ethanolate, DRV) |
Prezista |
June 23, 2006 |
fosamprenavir
(fosamprenavir calcium, FOS-APV, FPV) |
Lexiva |
October 20, 2003 |
ritonavir
(RTV) *Although ritonavir is a PI, it is generally used as a pharmacokinetic enhancer as recommended in the Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV and the Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection. |
Norvir |
March 1, 1996 |
tipranavir
(TPV) |
Aptivus |
June 22, 2005 |
| Fusion Inhibitors |
| Fusion inhibitors block HIV from entering the CD4 T lymphocyte (CD4 cells) of the immune system. |
enfuvirtide
(T-20) |
Fuzeon |
March 13, 2003 |
| CCR5 Antagonists |
| CCR5 antagonists block CCR5 coreceptors on the surface of certain immune cells that HIV needs to enter the cells. |
maraviroc
(MVC) |
Selzentry |
August 6, 2007 |
| Integrase Strand Transfer Inhibitor (INSTIs) |
| Integrase inhibitors block HIV integrase, an enzyme HIV needs to make copies of itself. |
cabotegravir
(cabotegravir sodium, CAB) |
Vocabria |
January 22, 2021 |
dolutegravir
(dolutegravir sodium, DTG) |
Tivicay Tivicay PD |
August 12, 2013 June 12, 2020 |
raltegravir
(raltegravir potassium, RAL) |
Isentress |
October 12, 2007 |
| Isentress HD |
May 26, 2017 |
| Attachment Inhibitors |
| Attachment inhibitors bind to the gp120 protein on the outer surface of HIV, preventing HIV from entering CD4 cells. |
fostemsavir
(fostemsavir tromethamine, FTR) |
Rukobia |
July 2, 2020 |
| Post-Attachment Inhibitors |
| Post-attachment inhibitors block CD4 receptors on the surface of certain immune cells that HIV needs to enter the cells. |
ibalizumab-uiyk
(Hu5A8, IBA, Ibalizumab, TMB-355, TNX-355) |
Trogarzo |
March 6, 2018 |
| Capsid Inhibitors |
| Capsid inhibitors interfere with the HIV capsid, a protein shell that protects HIV's genetic material and enzymes needed for replication. |
lenacapavir
(GS-6207, GS-HIV, GS-CA2, GS-CA1) |
Sunlenca |
December 22, 2022 |
| Pharmacokinetic Enhancers |
| Pharmacokinetic enhancers are used in HIV treatment to increase the effectiveness of an HIV medicine included in an HIV treatment regimen. |
cobicistat
(COBI, c) |
Tybost |
September 24, 2014 |
| Combination HIV Medicines |
| Combination HIV medicines contain two or more HIV medicines from one or more drug classes. |
abacavir and lamivudine
(abacavir sulfate / lamivudine, ABC / 3TC) |
Epzicom |
August 2, 2004 |
| abacavir, dolutegravir, and lamivudine(abacavir sulfate / dolutegravir sodium / lamivudine, ABC / DTG / 3TC) |
Triumeq |
August 22, 2014 |
| Triumeq PD |
March 30, 2022 |
abacavir, lamivudine, and zidovudine
(abacavir sulfate / lamivudine / zidovudine, ABC / 3TC / ZDV) |
Trizivir |
November 14, 2000 |
atazanavir and cobicistat
(atazanavir sulfate / cobicistat, ATV / COBI) |
Evotaz |
January 29, 2015 |
bictegravir, emtricitabine, and tenofovir alafenamide
(bictegravir sodium / emtricitabine / tenofovir alafenamide fumarate, BIC / FTC / TAF) |
Biktarvy |
February 7, 2018 |
cabotegravir and rilpivirine
(CAB and RPV, CAB plus RPV, Cabenuva kit, cabotegravir extended-release injectable suspension and rilpivirine extended-release injectable suspension) |
Cabenuva |
January 22, 2021 |
darunavir and cobicistat
(darunavir ethanolate / cobicistat, DRV / COBI) |
Prezcobix |
January 29, 2015 |
darunavir, cobicistat, emtricitabine, and tenofovir alafenamide
(darunavir ethanolate / cobicistat / emtricitabine / tenofovir AF, darunavir ethanolate / cobicistat / emtricitabine / tenofovir alafenamide, darunavir / cobicistat / emtricitabine / tenofovir AF, darunavir / cobicistat / emtricitabine / tenofovir alafenamide fumarate, DRV / COBI / FTC / TAF) |
Symtuza |
July 17, 2018 |
dolutegravir and lamivudine
(dolutegravir sodium / lamivudine, DTG / 3TC) |
Dovato |
April 8, 2019 |
dolutegravir and rilpivirine
(dolutegravir sodium / rilpivirine hydrochloride, DTG / RPV) |
Juluca |
November 21, 2017 |
doravirine, lamivudine, and tenofovir disoproxil fumarate
(doravirine / lamivudine / TDF, doravirine / lamivudine / tenofovir DF, DOR / 3TC / TDF) |
Delstrigo |
August 30, 2018 |
efavirenz, emtricitabine, and tenofovir disoproxil fumarate
(efavirenz / emtricitabine / tenofovir DF, EFV / FTC / TDF) |
Atripla |
July 12, 2006 |
efavirenz, lamivudine, and tenofovir disoproxil fumarate
(EFV / 3TC / TDF) |
Symfi |
March 22, 2018 |
efavirenz, lamivudine, and tenofovir disoproxil fumarate
(EFV / 3TC / TDF) |
Symfi Lo |
February 5, 2018 |
elvitegravir, cobicistat, emtricitabine, and tenofovir alafenamide
(elvitegravir / cobicistat / emtricitabine / tenofovir alafenamide fumarate, EVG / COBI / FTC / TAF) |
Genvoya |
November 5, 2015 |
elvitegravir, cobicistat, emtricitabine, and tenofovir disoproxil fumarate
(QUAD, EVG / COBI / FTC / TDF) |
Stribild |
August 27, 2012 |
emtricitabine, rilpivirine, and tenofovir alafenamide
(emtricitabine / rilpivirine / tenofovir AF, emtricitabine / rilpivirine / tenofovir alafenamide fumarate, emtricitabine / rilpivirine hydrochloride / tenofovir AF, emtricitabine / rilpivirine hydrochloride / tenofovir alafenamide, emtricitabine / rilpivirine hydrochloride / tenofovir alafenamide fumarate, FTC / RPV / TAF) |
Odefsey |
March 1, 2016 |
emtricitabine, rilpivirine, and tenofovir disoproxil fumarate
(emtricitabine / rilpivirine hydrochloride / tenofovir disoproxil fumarate, emtricitabine / rilpivirine / tenofovir, FTC / RPV / TDF) |
Complera |
August 10, 2011 |
emtricitabine and tenofovir alafenamide
(emtricitabine / tenofovir AF, emtricitabine / tenofovir alafenamide fumarate, FTC / TAF) |
Descovy |
April 4, 2016 |
emtricitabine and tenofovir disoproxil fumarate
(emtricitabine / tenofovir DF, FTC / TDF) |
Truvada |
August 2, 2004 |
lamivudine and tenofovir disoproxil fumarate
(3TC / TDF) |
Cimduo |
February 28, 2018 |
lamivudine and zidovudine
(3TC / ZDV) |
Combivir |
September 27, 1997 |
lopinavir and ritonavir
(ritonavir-boosted lopinavir, LPV/r, LPV / RTV) |
Kaletra |
September 15, 2000 |