Key Points
- Long-acting HIV medicines have become increasingly popular in recent years, offering a safe way to reduce how often someone needs to take HIV medicines.
- Long-acting HIV medicines are injected under the supervision of a health care provider rather than taken as an oral pill at home.
- Unlike most oral HIV medicines that are taken daily, long-acting HIV medicines are injected on schedules ranging from every two weeks to every six months, depending on the medicine.
What are long-acting HIV medicines?
Long-acting HIV medicines are HIV medicines that stay in the body for a longer period of time. Since long-acting HIV medicines stay in the body longer, they can be taken less frequently.
Some of the most common long-acting HIV medicines include—
As of 2025, these are the only long-acting medicines that are approved by the U.S. Food and Drug Administration (FDA) for HIV prevention or treatment. This fact sheet focuses on HIV treatment. View the HIVinfo Pre-Exposure Prophylaxis fact sheet to learn more about long-acting medicines for HIV prevention.
How are long-acting HIV medicines different?
Long-acting HIV medicines are unique because they can maintain stable concentrations in the body for much longer than most oral HIV medicines. As a result, this means that people who use long-acting HIV medicines don’t have to take pills for each HIV medicine in their treatment regimen every day.
Instead of taking pills every day, long-acting HIV medicines are injected much less frequently. For example, the FDA-approved long-acting HIV medicines are usually taken on the following schedule—
- Cabenuva – Every one or two months
- Sunlenca – Every six months
- Trogarzo – Every two weeks
Unlike HIV medicines in pill form, long-acting HIV medicines must be given at an appointment with a health care provider. Some research shows that long-acting HIV medicines could help people who struggle to take pills frequently, known as medication adherence.
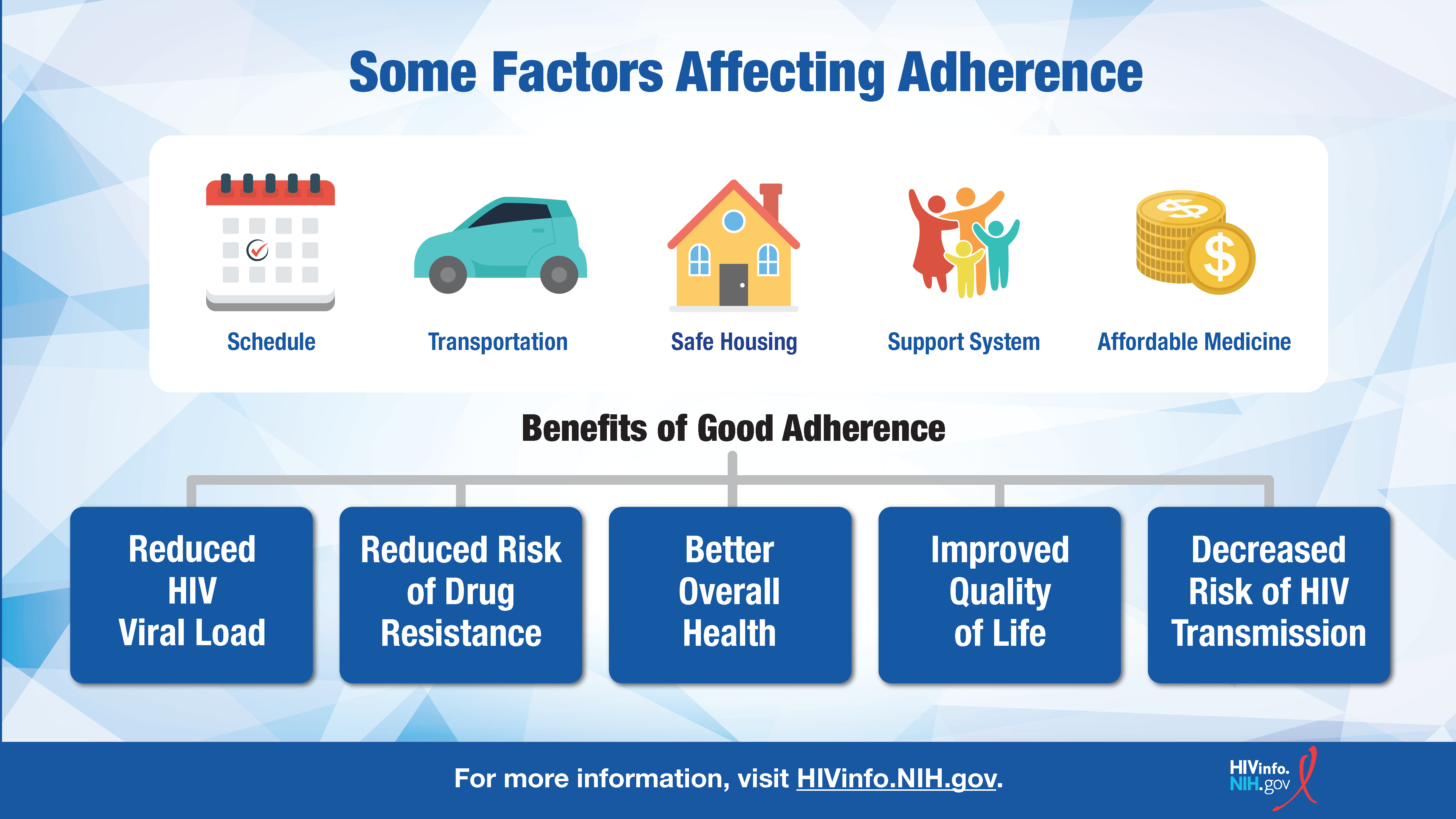
Medication adherence is critical for HIV medicines to be fully effective. Because long-acting HIV medicines can help overcome some barriers related to adherence, additional long-acting medicines are being investigated for HIV prevention and treatment. The HIV Treatment Adherence fact sheet provides more information on factors that may affect adherence.
Although long-acting HIV medicines can be taken less frequently, sometimes other HIV medicines must still be taken every day. For instance, Sunlenca is only taken every six months, but it is used to supplement other HIV medicines in your treatment regimen.
Are long-acting HIV medicines safe?
Long-acting HIV medicines, like other FDA-approved HIV medicines, are considered safe for most people. All medicines have the potential for some side effects. For long-acting HIV medicines, the most common side effects include:
- Diarrhea
- Dizziness
- Fatigue
- Fever
- Headache
- Nausea
- Rash
- Sleep problems
- Soreness, swelling, or redness around the injection site
Less commonly, long-acting HIV medicines can cause more serious side effects like depression or liver problems. However, serious side effects are rare and usually can be avoided by communicating with your health care provider before taking a new HIV medicine.
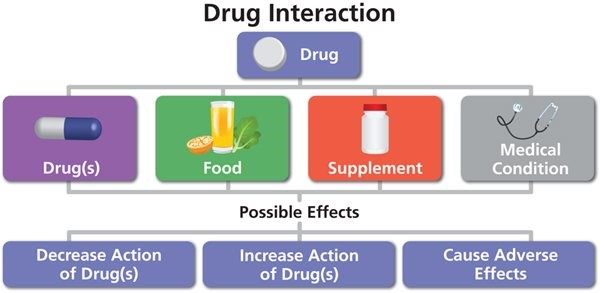
In addition, many HIV medicines (including long-acting HIV medicines) may be prone to drug interactions if combined with other drugs, including over-the-counter drugs. For example, long-acting HIV medicines may interact with some antibiotics and anticonvulsants.
Lastly, there are not enough data to guarantee that these medicines are safe to use during pregnancy or while breastfeeding. Although it is possible that these medicines are safe in these scenarios, they are not recommended in such cases due to a lack of data. A health care provider should help select HIV medicines based on your unique personal situation.
Should I switch to a long-acting HIV medicine?
Switching HIV medicines should occur only after consultation with a health care provider. In some cases, there will be no need to switch an HIV treatment regimen if it is working effectively and you can tolerate the current dosing schedule. Switching HIV treatment regimens may lead to drug resistance, which could limit treatment options in the future.
In addition, there are only a few long-acting HIV medicines available to choose from, with some options reserved for unique situations. For example, Trogarzo is typically prescribed when a person is resistant to multiple classes of HIV medicines. When this happens, normal HIV medicines do not work effectively, and Trogarzo is used like an emergency medicine.
There are some cases when it is beneficial to switch to a long-acting HIV medicine. For example, if you are struggling to keep up with the demands of taking pills every day, long-acting HIV medicines could be more effective.
In addition, other factors that could affect your ability to take long-acting HIV medicines should be addressed. These medicines may have different costs or side effects that might not meet your needs or preferences.
If you believe you are a good candidate for a long-acting HIV medicine, it is possible you could be eligible to participate in a clinical trial. Always consult your health care provider about taking any new medicines and any concerns related to an HIV treatment regimen. For more information about clinical trials, see the HIVinfo HIV and AIDS Clinical Trials and What is an Investigational HIV Drug? fact sheets.
This fact sheet is based on information from the following sources:
From the National Institutes of Health:
From CDC:
From the World Health Organization:
Also see the HIV Source collection of HIV links and resources.