HIV and Gay and Bisexual Men
Key Points
- In the United States, gay and bisexual men are the population group most affected by HIV.
- The Centers for Disease Control and Prevention (CDC) recommends that all sexually active gay and bisexual men get tested for HIV at least once a year. However, some sexually active gay and bisexual men who have multiple sex partners or casual sex with people whose status is unknown may benefit from getting tested more often (for example, every 3 to 6 months).
- Gay and bisexual men who are HIV negative but at risk of getting HIV should consider pre-exposure prophylaxis (PrEP). PrEP is when people who do not have HIV but who are at risk of getting HIV take HIV medicine every day (pills) or every two months (an injection) to reduce their chances of HIV infection. The CDC reports that PrEP is highly effective for preventing HIV from sex or injection drug use.
Does HIV affect gay and bisexual men?
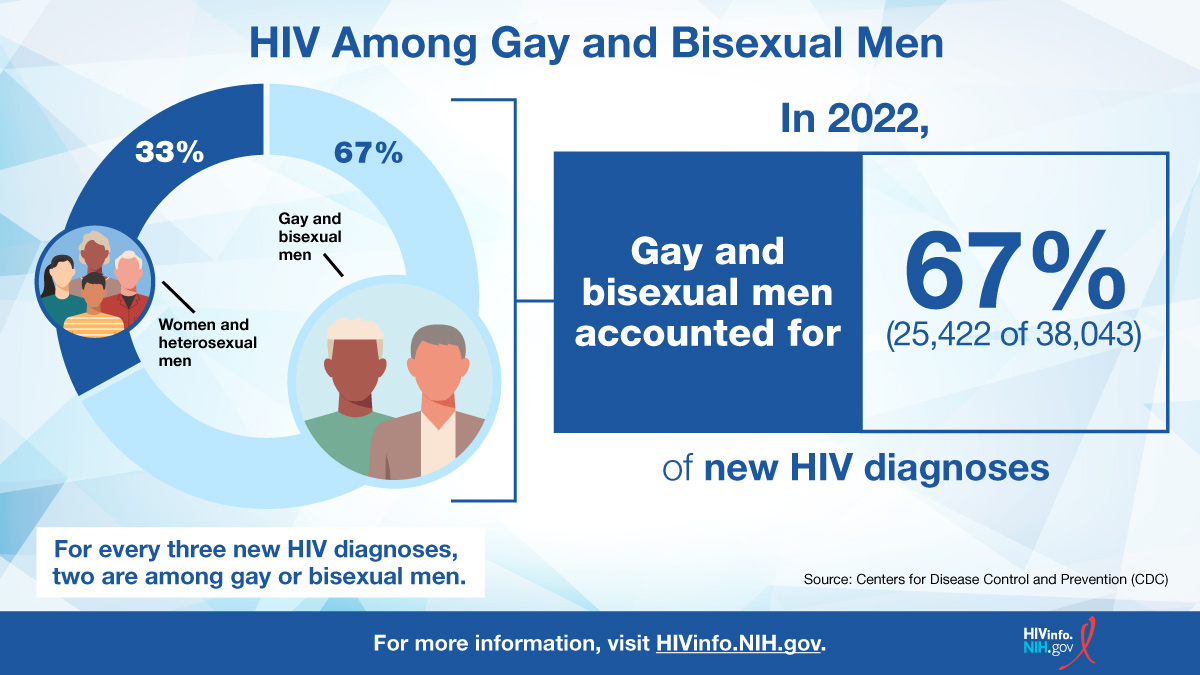
In the United States, gay and bisexual men are the population most affected by HIV. According to the Centers for Disease Control and Prevention (CDC), in 2022, adult and adolescent gay, bisexual, and other men who reported male-to-male sexual contact accounted for 67% of the new HIV diagnoses in the United States and dependent areas.
What factors put gay and bisexual men at risk for HIV infection?
Factors that put gay and bisexual men at risk for HIV infection:
- Male-to-male sexual contact. Of all new HIV diagnoses in the United States, 67% were among gay, bisexual, and other men who reported male-to-male sexual contact. This high percentage of all men who have male-to-male sexual contact and have HIV means that, as a group, they have a greater likelihood of being exposed to HIV.
- Having sex without using an HIV prevention strategy. Most gay and bisexual men get HIV from having anal sex without using condoms or without taking medicines to prevent or treat HIV (see PrEP below). Anal sex is the riskiest type of sex for getting HIV or passing it on to others (called HIV transmission).
- Homophobia, stigma, and discrimination. Negative attitudes about homosexuality may discourage gay and bisexual men from getting tested for HIV and finding health care to prevent and treat HIV.
What steps can gay and bisexual men take to prevent HIV infection?
Gay and bisexual men can take the following steps to reduce their risk of HIV infection:
Choose less risky sexual behaviors.
Anal sex is the riskiest type of sex for getting or transmitting HIV. Receptive anal sex (bottoming) is 13 times riskier for getting HIV than insertive anal sex (topping).
In general, oral sex has a low risk of transmitting HIV. However, it is hard to know the exact risk because a lot of people who have oral sex also have anal or vaginal sex. Other sexually transmitted infections (STIs), such as syphilis, herpes, gonorrhea, and chlamydia, can be transmitted during oral sex.
Limit your number of sex partners.
The more partners you have, the more likely you are to have a partner with poorly controlled HIV or to have a partner with an STI. Both factors can increase the likelihood of HIV transmission. Having an STI may create inflammation or open sores that make it easier for HIV to penetrate your skin. Syphilis, which is especially prevalent among men who have sex with men, can put you at high risk for HIV in the future.
Use condoms correctly every time you have sex.
Read this CDC fact sheet on the proper way to use condoms: Male (External) Condom Use.
Consider pre-exposure prophylaxis (PrEP).
Pre-exposure prophylaxis (PrEP) is HIV medicine taken to reduce the chances of getting HIV infection. PrEP is used by people who do not have HIV but are at high risk of being exposed to HIV. PrEP can be taken as an oral medicine (pills) or delivered as a long-acting injection once every two months. PrEP can be combined with other prevention methods, such as condoms, to reduce the risk of HIV even further. To learn more, read the HIVinfo fact sheet on Pre-Exposure Prophylaxis (PrEP).
Consider post-exposure prophylaxis (PEP).
Post-exposure prophylaxis (PEP) is the use of HIV medicines soon after a possible exposure to HIV to prevent becoming infected with HIV. For example, a person who is HIV negative may use PEP after having sex without a condom with a person who is HIV positive. To be effective, PEP must be started within 72 hours after a possible exposure to HIV.
PEP is for emergency situations. It is not a substitute for PrEP or the regular use of other HIV prevention methods.
To learn more, read the HIVinfo fact sheet on Post-Exposure Prophylaxis (PEP).
Get tested for HIV.
Whether you test HIV positive or HIV negative, in both cases you can take action to protect your health and prevent HIV transmission.
How often is HIV testing recommended for gay and bisexual men?
The CDC recommends that all sexually active gay, bisexual, and other men who have male-to-male sexual contact get tested for HIV at least once a year. However, some sexually active gay and bisexual men (such as those who have more than one partner or have had casual sex with people they do not know) may benefit from getting tested more often (for example, every 3 to 6 months).
Visit this CDC webpage to learn more about HIV testing and to find a testing location near you: Let’s Stop HIV Together.
How should a gay man living with HIV protect his partner from HIV?
Take HIV medicines every day as prescribed by your health care provider. Treatment with HIV medicines (called antiretroviral therapy or ART) is recommended for everyone who has HIV. ART cannot cure HIV infection, but it can reduce the amount of HIV in the body (called the viral load).
A main goal of ART is to reduce a person’s viral load to an undetectable level. An undetectable viral load means that the level of HIV in the blood is too low to be detected by a viral load test.
- People with HIV whose viral load stays undetectable have effectively no risk of transmitting HIV to an HIV-negative partner through sex.
- Maintaining an undetectable viral load is also the best way to stay healthy. Recent studies have shown that delaying treatment can increase the chances that people living with HIV will develop AIDS and other serious illnesses.
Other steps you can take include using condoms during sex and talking to your partner about taking PrEP.
This fact sheet is based on information from the following sources:
From CDC:
- HIV Surveillance Report, 2021
- HIV and Gay and Bisexual Men
- Preventing HIV With PrEP
- Preventing HIV With PEP
- Preventing HIV
- Safer Sex 101 for HIV (PDF)
Also see the HIV Source collection of HIV links and resources.