HIV and Women
Key Points
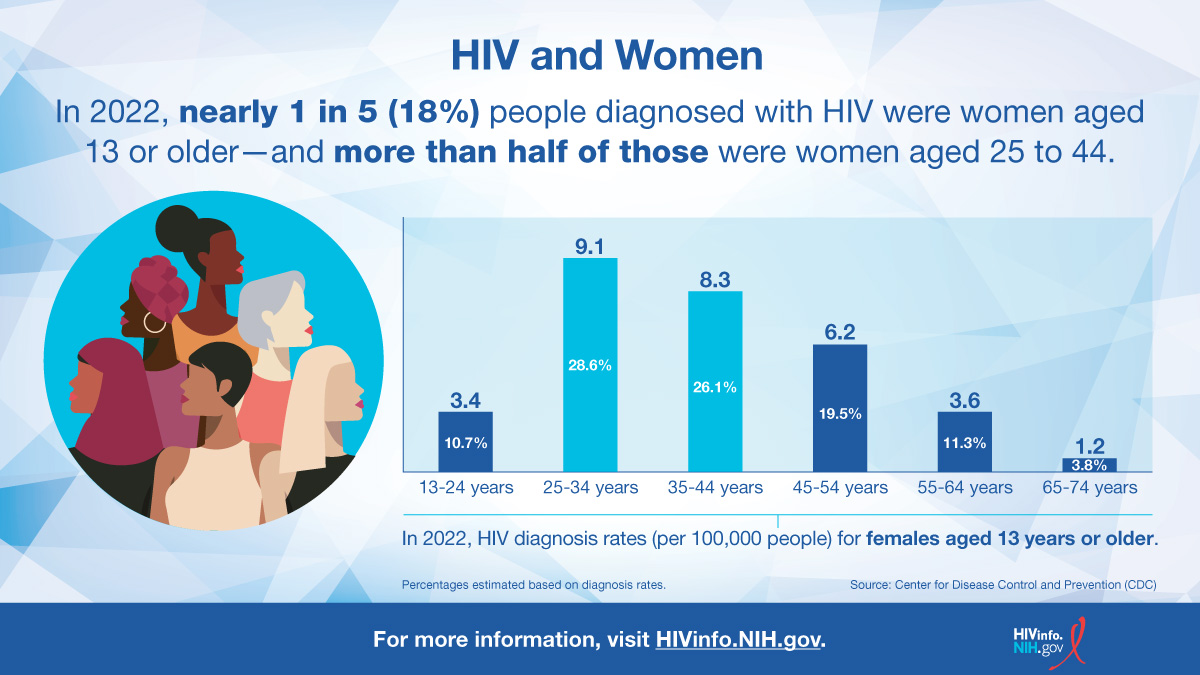
- According to the Centers for Disease Control and Prevention (CDC), in 2022, 18% of the new HIV diagnoses in the United States and dependent areas were among women.
- The most common way that women get HIV is through sex with a male partner who has HIV. During vaginal or anal sex, a woman has a greater risk for getting HIV because, in general, receptive sex is riskier than insertive sex.
- Women with HIV take HIV medicines during pregnancy and childbirth to prevent perinatal transmission of HIV and to protect their own health.
Does HIV affect women?
Yes. According to the Centers for Disease Control and Prevention (CDC), in 2022, 18% of the new HIV diagnoses in the United States and dependent areas were among women. In addition, 56% of women with HIV are Black/African American.
The most common way that women get HIV is through sex with a male partner who has HIV without using condom. Most women who have HIV know that they are HIV positive, but some women are not getting the HIV care and treatment they need.
What factors put women at risk for HIV?
HIV can be transmitted from one person to another through bodily fluids such as blood, pre-seminal fluids, semen, vaginal fluids, rectal fluids, and breast milk. In the United States, the main risk factors for HIV transmission are the following:
- Having anal or vaginal sex with a person who has HIV without using a condom or taking medicines to prevent or treat HIV. Anal sex is the riskiest type of sex for getting HIV, because the rectum’s lining is thin and may allow HIV to enter the body during anal sex.
- Sharing injection drug equipment (works), such as needles, with a person who has HIV
In women, several factors can increase the risk of HIV transmission. For example, during vaginal or anal sex, a woman has a greater risk for getting HIV because, in general, receptive sex is riskier than insertive sex. Age-related thinning and dryness of the vagina may also increase the risk of HIV in older women, because these can cause a tear in the vagina during sex and lead to HIV transmission. A woman’s risk of HIV can also increase if her partner engages in high-risk behaviors, such as injection drug use or having sex with other partners without using condoms.
Are there any issues that affect HIV treatment in women?
Treatment with HIV medicines (called antiretroviral therapy or ART) is recommended for everyone with HIV. Treatment with HIV medicines helps people with HIV live long, healthy lives. ART also reduces the risk of HIV transmission.
People should start taking HIV medicines as soon as possible after HIV is diagnosed. However, birth control and pregnancy are two issues that can affect HIV treatment in women.
Birth control
Some HIV medicines may reduce the effectiveness of hormonal contraceptives, such as birth control pills, patches, rings, or implants. Women taking certain HIV medicines may have to use an additional or different form of birth control. For more information, view the HIV and Birth Control infographic from HIVinfo.
Pregnancy
Women with HIV take HIV medicines during pregnancy and childbirth to reduce the risk of perinatal transmission of HIV and to protect their own health. See the Preventing Perinatal Transmission fact sheet for more information.
The choice of an HIV treatment regimen to use during pregnancy depends on several factors, including a woman’s current or past use of HIV medicines, other medical conditions she may have, and the results of drug-resistance testing. In general, pregnant women with HIV can use the same HIV treatment regimens recommended for non-pregnant adults—unless the risk of any known side effects to a pregnant woman or her baby outweighs the benefits of a regimen.
Sometimes a woman’s HIV treatment regimen may change during pregnancy. Women and their health care providers should discuss whether any changes need to be made to an HIV treatment regimen during pregnancy.
PrEP and PEP for women
Pre-exposure prophylaxis (PrEP) is HIV medicine taken to reduce the chances of getting HIV infection. PrEP is used by people who do not have HIV but are at high risk of being exposed to HIV through sex or injection drug use.
There are two PrEP medications approved for use by women:
- Truvada (or a generic equivalent), a pill that is taken by mouth every day.
- Apretude, a shot that is taken every 2 months.
In emergency situations, people can also take post-exposure prophylaxis (PEP). PEP is HIV medicine taken within 72 hours (3 days) to reduce the chances of getting HIV infection after a possible exposure to HIV.
Women should speak with their health care provider to learn about PrEP and PEP and how to protect themselves from HIV. See the Pre-Exposure Prophylaxis (PrEP) and Post-Exposure Prophylaxis (PEP) fact sheets for more detailed information about PrEP and PEP.
This fact sheet is based on information from the following sources:
From CDC:
From the Department of Health and Human Services:
- Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV:
- Recommendations for the Use of Antiretroviral Drugs During Pregnancy and Interventions to Reduce Perinatal HIV Transmission in the United States:
- Office on Women's Health:
Also see the HIV Source collection of HIV links and resources.