The HIV Life Cycle
Key Points
- HIV damages the immune system by infecting and destroying CD4 cells (CD4 T lymphocytes), which protect the body from infection.
- HIV uses CD4 cells to multiply and spread through the body in a seven-step process known as the HIV life cycle. HIV medicines protect the immune system by blocking HIV at different stages of the HIV life cycle.
- Antiretroviral therapy (ART) is the use of a combination of HIV medicines from at least two different drug classes to treat HIV. Because each class of drugs is designed to target a specific step in the HIV life cycle, ART is very effective at preventing HIV from multiplying.
What is the HIV life cycle?
Viruses cannot multiply by themselves. They must enter and take over the target cells to make copies of the virus. The multiple steps involved in virus multiplication occur inside the infected cells and are collectively termed the “virus life cycle.”
HIV can recognize and infect the CD4 cells (CD4 T lymphocytes) of the immune system, destroying many of these cells in the process. CD4 cells are a type of white blood cell that help protect the body from infection with viruses, bacteria, and fungi. HIV uses components of the CD4 cells to multiply in large numbers and spread throughout the body.
What are the seven stages of the HIV life cycle?
The HIV virus is very small at about 100 nanometers in diameter (about one-thousandth of the thickness of a regular sheet of paper). Despite its small size, the virus is composed of multiple components that are essential to its progression through the HIV life cycle, such as the capsid and envelope.
Figure 1. Structure of an HIV Particle
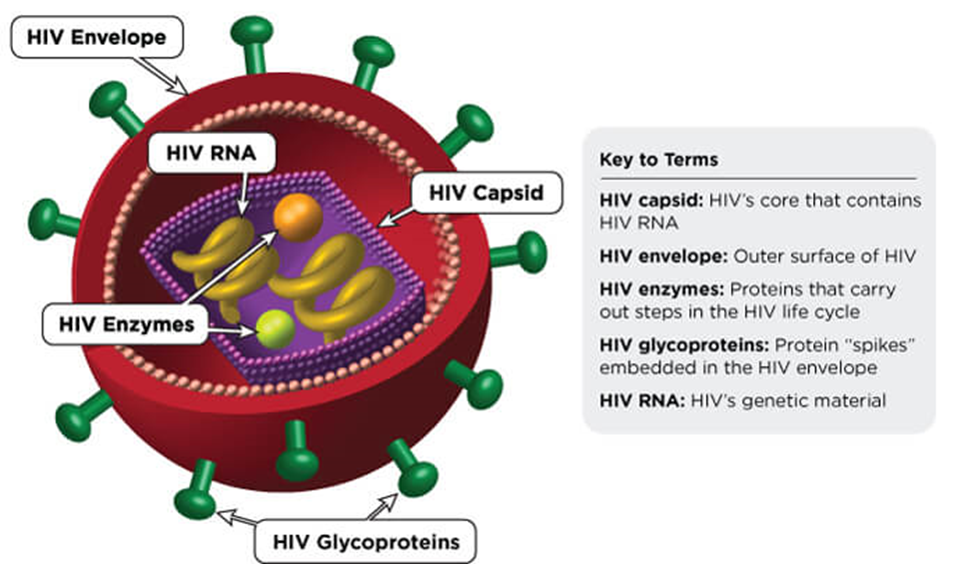
The various components of the HIV particle each play an important role in the HIV life cycle, allowing the particle to infect CD4 cells and make more copies of the virus. The seven stages of the HIV life cycle are:
- Binding: HIV binds to receptors on the surface of a CD4 cell.
- Fusion: The HIV envelope fuses with the CD4 cell membrane, allowing HIV to enter the CD4 cell.
- Reverse transcription: Inside the CD4 cell, HIV releases and uses reverse transcriptase (an HIV enzyme) to convert its genetic material (HIV RNA) into HIV DNA. This allows HIV to enter the CD4 cell nucleus.
- Integration: Inside the CD4 cell nucleus, HIV integrase (an HIV enzyme) helps HIV integrate its viral DNA into the DNA of the CD4 cell.
- Replication: Once integrated into the DNA of the CD4, HIV uses parts of the CD4 cell to create long chains of HIV proteins, allowing HIV to build more and more particles.
- Assembly: New HIV proteins (from the replication stage) and HIV RNA move to the surface of the cell and assemble into immature (non-infectious) HIV.
- Budding: Newly formed immature HIV pushes itself out of the host CD4 cell. New HIV then releases protease (an HIV enzyme) to break apart protein chains in the immature virus, creating a mature (infectious) virus.
Figure 2. Stages of the HIV Life Cycle
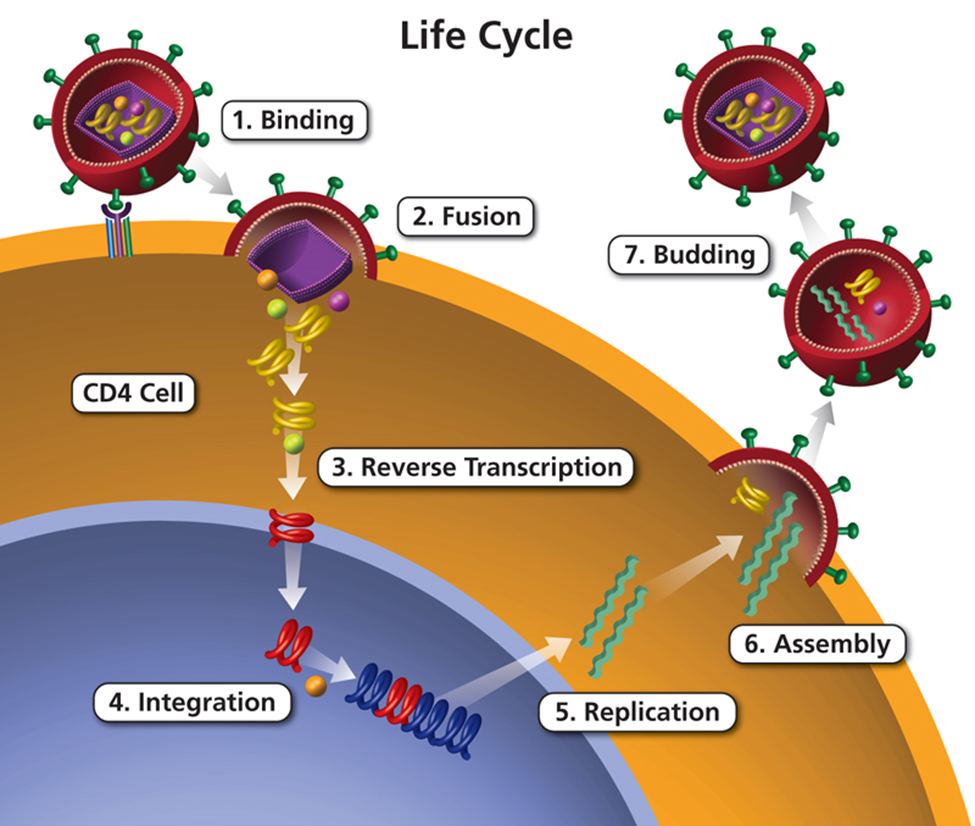
It is reported that during the acute stage of HIV infection, about 10,000 new HIV particles can be produced from one CD4 cell, resulting in an increase in the number of infected CD4 cells.
What is the connection between the HIV life cycle and HIV medicines?
Research scientists design drugs that target specific stages of the HIV life cycle to obstruct or block the virus from multiplying to prevent damage to CD4 cells. As a result, the number of CD4 cells remains high and the person with HIV maintains normal immune function.
Antiretroviral therapy (ART) typically includes a combination of HIV medicines from different drug classes (at least two) to treat HIV infection. People on ART take a combination of HIV medicines (called an HIV treatment regimen) every day (pills) or every one or two months (injections). HIV medicines from different drug classes protect the immune system by blocking HIV at different stages of the HIV life cycle.
Because an HIV treatment regimen includes HIV medicines from at least two different HIV drug classes, ART is very effective at blocking the virus and preventing HIV from multiplying in large numbers.
| Drug Class | Example | Mechanism | HIV Life Cycle Stage |
|---|---|---|---|
| Entry Inhibitors | Maraviroc, fostemsavir | Block HIV from entering the host cell by preventing the virus from binding to the cell surface. | Binding (or attachment) |
| Fusion Inhibitors | Enfuvirtide | Prevent the HIV envelope from fusing with the CD4 cell membrane, preventing the virus from entering the cell. | Fusion |
| Nucleoside Reverse Transcriptase Inhibitors (NRTIs) | Lamivudine, emtricitabine | Prevent HIV from converting its RNA into DNA, which is necessary for the virus to replicate. | Reverse Transcription |
| Non-Nucleoside Reverse Transcriptase Inhibitors (NNRTIs) | Rilpivirine, efavirenz | Bind to and inhibit the reverse transcriptase enzyme, stopping the conversion of RNA to DNA. | Reverse Transcription |
| Integrase Strand Transfer Inhibitors (INSTIs) | Dolutegravir, raltegravir | Block the HIV enzyme integrase, preventing the viral DNA from integrating into the host cell’s DNA. | Integration |
| Capsid Inhibitors | Lenacapavir | Disrupt the capsid, a protein shell that encases the viral RNA, preventing the virus from assembling properly. | Assembly |
| Protease Inhibitors (PIs) | Darunavir, ritonavir | Inhibit the protease enzyme, which is needed to cut newly formed viral proteins into their active forms. | Budding |
Having less HIV in the body protects the immune system and prevents HIV from advancing to AIDS. While ART cannot cure HIV, it can help people with HIV live long, healthy lives. HIV medicines also reduce the risk of HIV transmission, preventing the spread of HIV to others.
This fact sheet is based on information from the following sources:
From the National Institute of Allergy and Infectious Diseases:
Also see the HIV Source collection of HIV links and resources.
