HIV and Children
Key Points
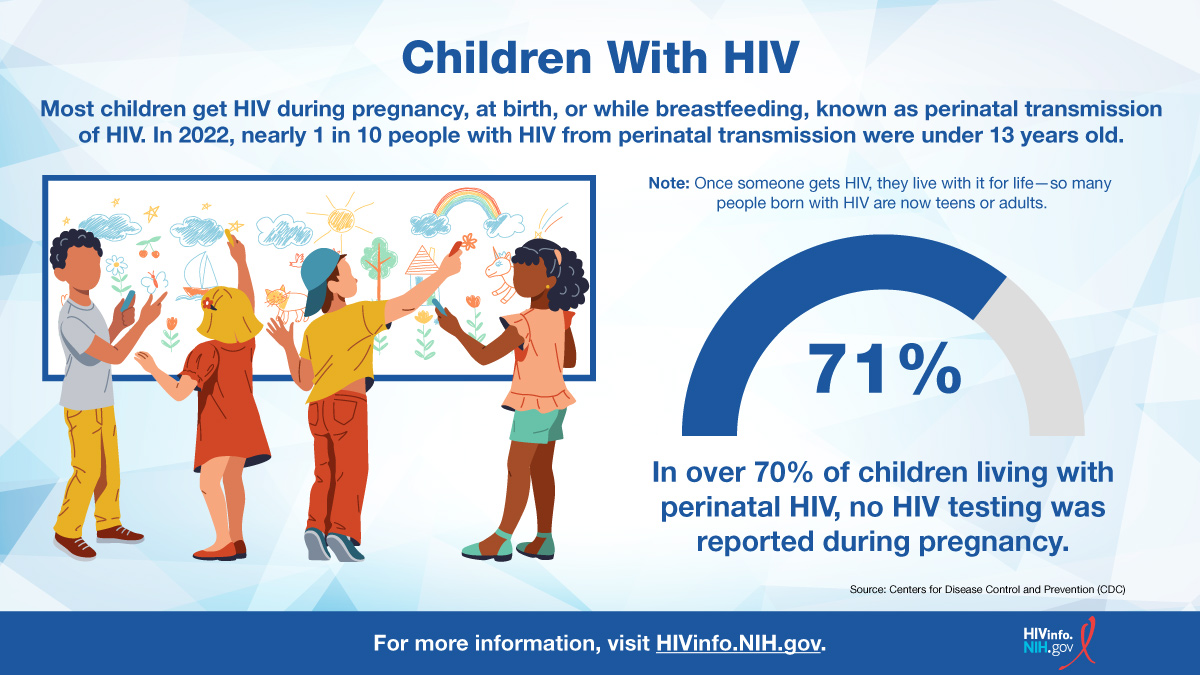
- Perinatal transmission: HIV can pass from a mother with HIV to their child during pregnancy, childbirth, or breastfeeding, called perinatal transmission of HIV. In the United States, this is the most common way children under 13 years of age get HIV. Perinatal transmission of HIV is also called mother-to-child transmission of HIV.
- HIV treatment: Several factors affect HIV treatment in children, including a child’s growth and development. For example, because children grow at different rates, dosing of an HIV medicine may depend on a child’s weight rather than their age.
- Treatment adherence: HIV medication adherence can be difficult for children. For example, a child may refuse to take HIV medicine because it tastes unpleasant.
Does HIV affect children?
Yes. According to the Centers for Disease Control and Prevention (CDC), 170 children younger than 13 years old were diagnosed with perinatally acquired HIV in the United States and Puerto Rico from 2018 to 2021. During this time, 12,139 children were born without HIV despite exposure to HIV during pregnancy, birth, or while breastfeeding.
How do most children get HIV?
HIV can pass from a mother with HIV to their child during pregnancy, childbirth, or breastfeeding, called perinatal transmission of HIV. In the United States, this is the most common way children under 13 years of age get HIV. Perinatal transmission of HIV is also called mother-to-child transmission of HIV.
The use of HIV medicines and other strategies have helped to lower the rate of perinatal transmission of HIV to 1% or less in the United States and Europe.
To learn more, read the HIVinfo fact sheets Preventing Perinatal Transmission of HIV and Preventing Perinatal Transmission of HIV After Birth.
What factors affect HIV treatment in children?
Treatment with HIV medicines (called antiretroviral therapy or ART) is recommended for everyone with HIV, including children. HIV medicines help people with HIV live long, healthy lives and reduce the risk of HIV transmission.
Several factors affect HIV treatment in children, including a child’s growth and development. For example, because children grow at different rates, dosing of an HIV medicine may depend on a child’s weight rather than their age. Children who are too young to swallow a pill may use HIV medicines that come in liquid form.
Issues that make it difficult to take HIV medicines every day and exactly as prescribed (called medication adherence) can affect HIV treatment in children. Effective HIV treatment depends on good medication adherence.
Why can medication adherence be difficult for children?
Several factors can make medication adherence difficult for children with HIV. For example, a child may refuse to take HIV medicine because it tastes unpleasant.
The following factors can also affect medication adherence in children:
- A busy parental schedule that makes it hard to take HIV medicines on time every day.
- Side effects from HIV medicines.
- Issues within a family, such as physical or mental illness, an unstable housing situation, or alcohol or drug abuse.
- Lack of health insurance to cover the cost of HIV medicines.
- A child’s age and developmental stage.
The HIVinfo fact sheet, Following an HIV Treatment Regimen: Steps to Take Before and After Starting HIV Medicines, includes tips on adherence. Some of the tips may be useful to children with HIV and their parents or caregivers.
This fact sheet is based on information from the following sources:
From CDC:
From the NIH Office of AIDS Research:
- Guidelines for the Use of Antiretroviral Agents in Pediatric HIV Infection:
- Recommendations for the Use of Antiretroviral Drugs During Pregnancy and Interventions to Reduce Perinatal HIV Transmission in the United States:
- Preventing Perinatal Transmission of HIV
- Preventing Perinatal Transmission of HIV After Birth.
Also see the HIV Source collection of HIV links and resources.
